Investigating biomarkers of migration and predictors of recurrence in glioblastoma
Using new surgical tools and AI to shed new light on glioblastoma recurrence
Glioblastoma (GBM) is an extremely aggressive type of brain cancer with a dismal five-year survival rate of just 5 per cent. Even after aggressive treatment—including surgery, radiation and chemotherapy—the cancer always returns, meaning that patients typically survive just 12 to 18 months past their initial diagnosis.
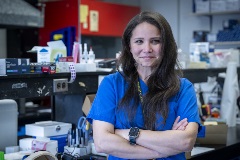
As a neurosurgeon and researcher at Queen’s University and the Kingston Health Sciences Centre, Dr. Teresa Purzner knows all too well about the difficulties to treat and study GBMs. That’s why she has worked with her research team to develop an innovative instrument known as a capsular biopsy tool, which is helping surgeons like her capture high-quality tissue samples from patients to enhance GBM research.
“Unlike standard biopsy forceps, which can miss critical regions of a tumour, the device works with pre-operative imaging to collect consistent samples that reflect the true complexity of the tumour,” she explains. “It has shown superior efficiency and consistency in sample collection in comparison to standard biopsy forceps.”
Using these newly acquired high-quality samples and $450,000 from a new Clinician-Scientist Award from the Marathon of Hope Cancer Centres Network, Dr. Purzner and her team will launch a new research project that utilizes a three-pronged approach to better understand glioblastomas with the hopes of finding new ways to stop recurrence.
Her three-year project will focus on:
- Identifying biomarkers of recurrence using advanced imaging paired with molecular analysis.
- Mapping tumour–brain interactions by studying gene activity across different regions.
- Leveraging artificial intelligence to recognize patterns that predict tumour invasion and recurrence.
“Funding from the Marathon of Hope Cancer Centres Network will allow us to integrate surgical innovation, molecular profiling, and AI, to try to reveal why glioblastomas spread so relentlessly — and find new ways to intervene more effectively,” she says. “If successful, our work could lead to more personalized brain tumour treatments, improving surgical precision and guiding post-operative care.”
Key Researcher
-
Teresa
ResearcherProject Leader
Purzner
Related News Item
-
Network names three outstanding early-career clinician-scientists as recipients of its 2025 Clinician-Scientist Awards
Drs. Teresa Purzner, Antoine Desilets and Simon Roy will each receive $450,000 ($225,000 from the Network and $225,000 in matching funds) to support groundbreaking research in precision oncology.
